Trends
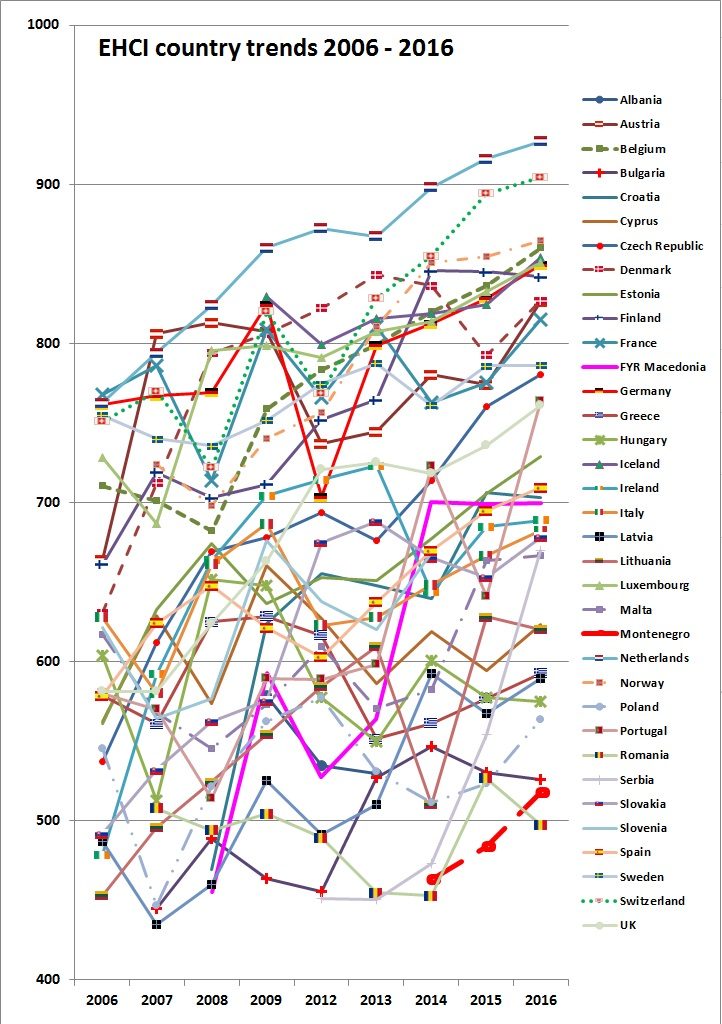
According to the EuroHealth Consumer Index 2017 the previous ten years have shown that European healthcare has been continuously improving also right through conditions such as the 2008 financial crisis. The Euro Health Consumer Index 2017 is an attempt at measuring and ranking the performance of healthcare provision from a consumer viewpoint. The Index displays consumer information, not medically or individually sensitive data. These results can serve as inspiration for how and where European healthcare can be improved.
From the point of view of a healthcare consumer, the overall situation is improving in most countries.
A feature, which was more prominent in post-crisis 2014 than in previous years is a stratification between affluent and less affluent countries. This gap is definitely less noticeable in 2016.
However, the performance of countries such as Portugal, FYR Macedonia and, in 2016, Serbia shows that GDP/capita need not be a dominating factor. Among the very few, where the 10-year trend over time is not rising, are countries as different as Sweden and Romania, plus Greece which seems to be recovering from a dive in 2012.
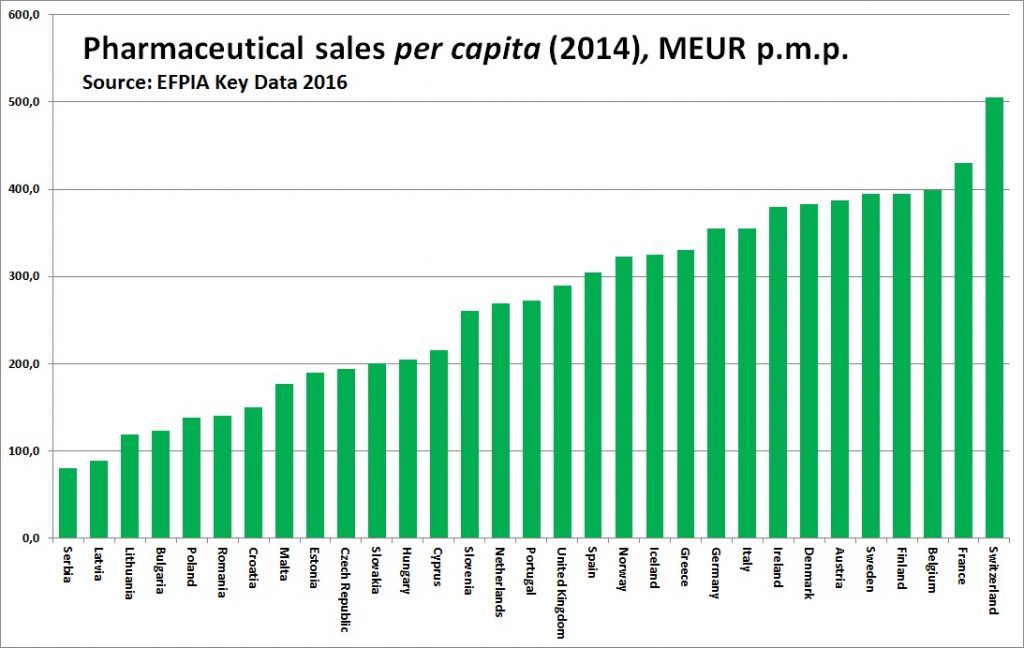
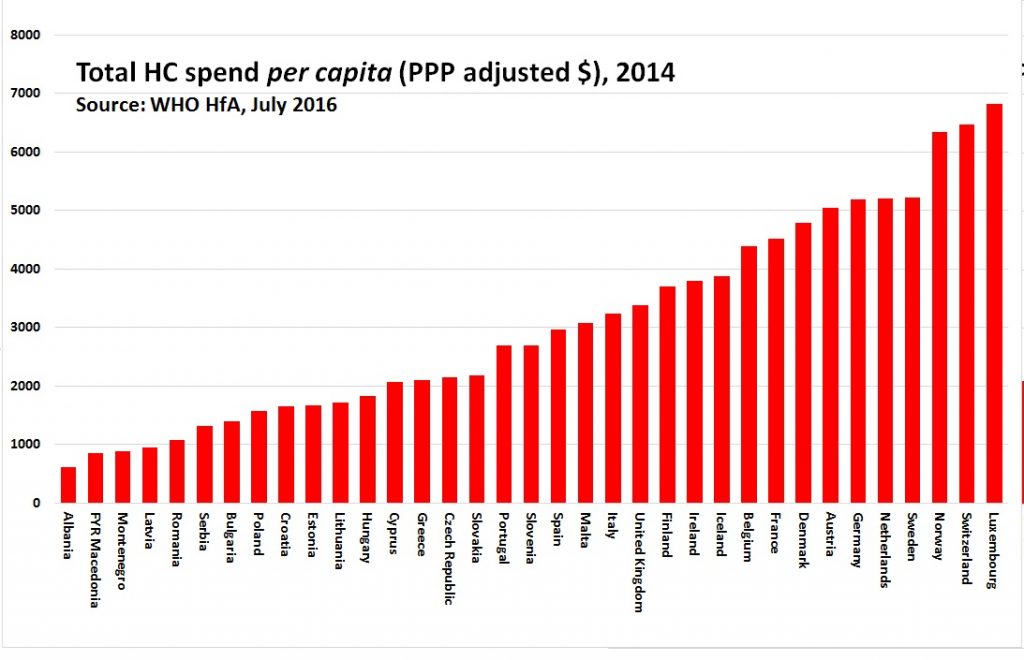 The correlation between money spent and healthcare performance is obvious for treatment results.
The correlation between money spent and healthcare performance is obvious for treatment results.
Romania today
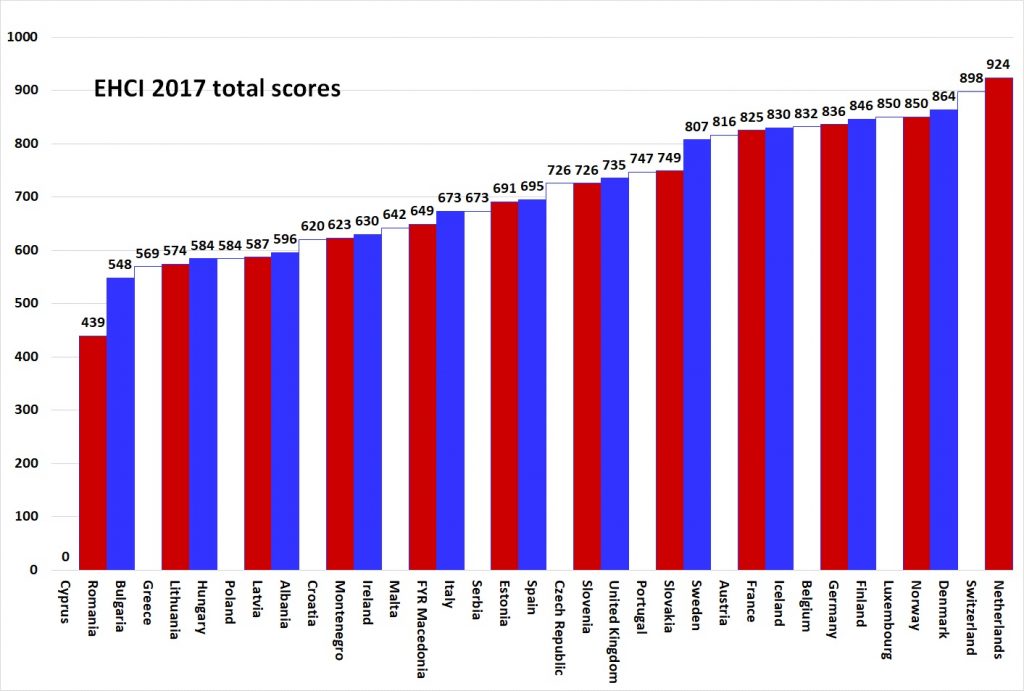
Romania is on the 34th place with 439 points.
Romania does have severe problems with the management of its entire public sector. In healthcare, discrimination of minority groups such as roma (3½ – 4% of the population) shows as poor Outcomes ratios, which in the EHCI 2017 is unfortunately punished harder than in previous editions.
Also, Albania, Romania and Bulgaria are suffering from an antiquated healthcare structure, with a high and costly ratio of in-patient care over out-patient care.
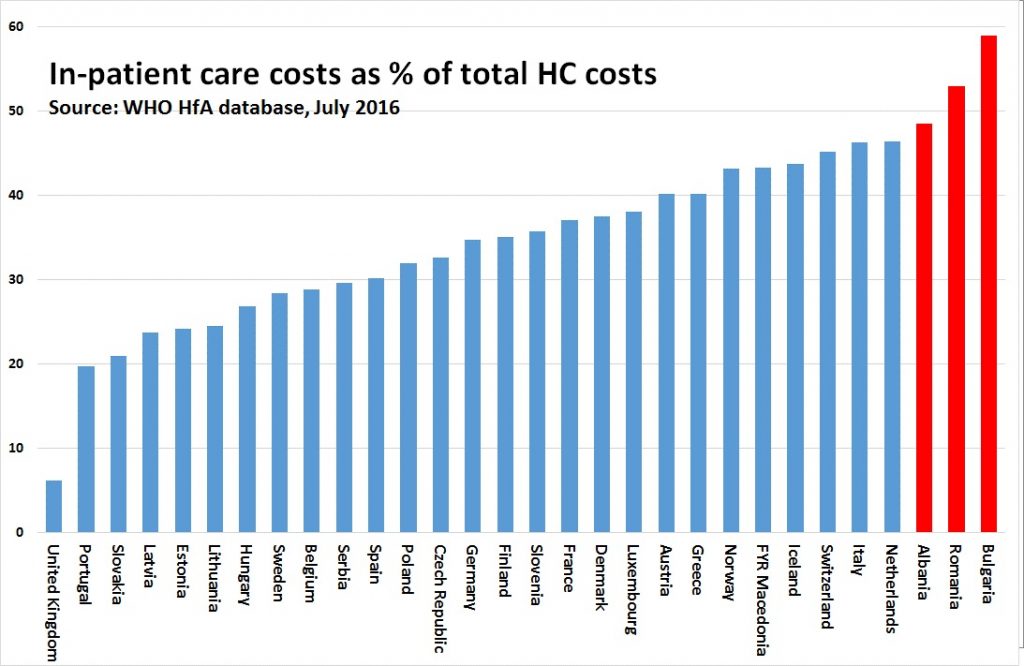
The higher the share of in-patient care, the more antiquated the healthcare provision structure. If Dutch, Swiss and (possibly) Italians prefer long hospital admissions, they can afford it; Bulgaria, Romania and Albania cannot! They should receive professional support to restructure their healthcare services!
The position of the Dutch healthcare system is to a great extent a product of an even performance across the sub-disciplines, very good medical quality and improved Accessibility, which used to be a weaker point in previous years.
Runner-up Switzerland is in top position for Accessibility, with Belgium. The Swedish healthcare system would be a real top contender, scoring high on Range & Reach of Services along with the NL, were it not for an accessibility situation, which by Belgian or Swiss standards can only be described as abysmal.

Total score

A comparative index for national healthcare systems has confirmed that there is a group of EU member states, which all have good healthcare systems seen from the customer/consumer’s point of view.
Some eastern European EU member systems are doing surprisingly well, particularly Slovakia, Slovenia, the Czech Republic and Estonia, considering their much smaller healthcare spend in Purchasing Power adjusted dollars per capita. However, readjusting from politically planned to consumer-driven economies does take time.
Romania scores the lowest in this category as Cyprus is very difficult to score in the EHCI, as Cyprus does not really have a public healthcare system in the general European meaning.
Informal payments to doctors
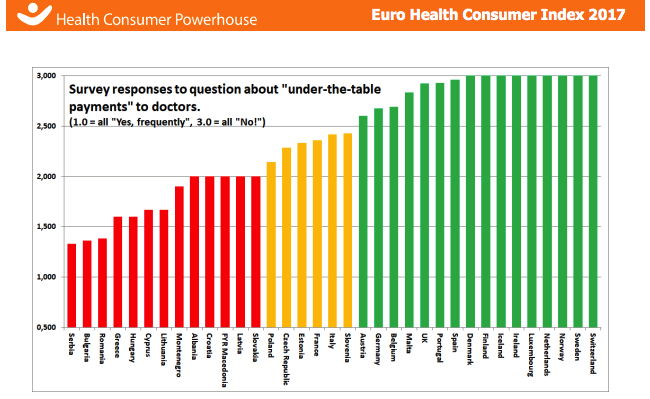
Mean response to question: “Would patients be expected to make unofficial payments?” with range of answers: plain “No!”, “Sometimes, depends on situation” and “Yes, frequently”. The indicator was first introduced in 2008. As an informal payment was considered any payment made by the patient in addition to official co-payment
In 2015, the countries fell in three fairly distinctive groups, making the R/Y/G scoring natural. These results have also been stable over the years, e.g. with Portugal and Spain scoring Green, and France and Austria scoring Yellow – in 2017, the Austrian score has made it into Green.
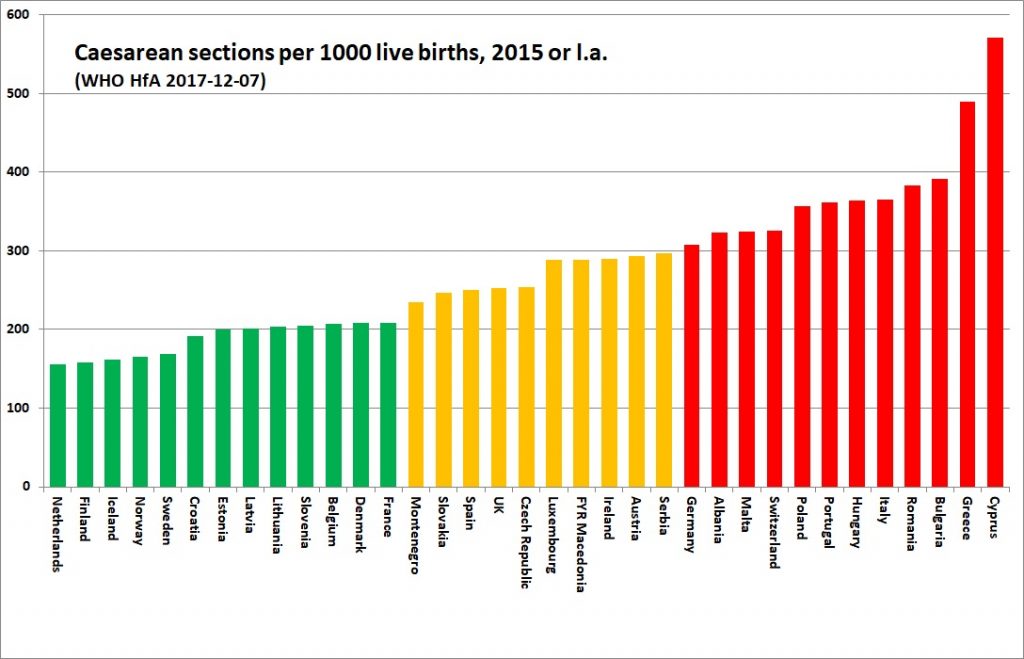
% of births by Caesarean section
Caesarean sections are associated with an increased risk of maternal death and puerperal complications, so use should be restricted to a few well-defined indications such as dangerous placental or foetal position. The World Health Organisation estimates that no more than 10 – 15% of deliveries are associated with a medically justifiable reason for a Caesarean section.
In scoring, it has been assumed that high Caesarean rates are an indication on poor pre-natal support and poor baby delivery services – consequently, a high Caesarean rate has been given a Red score. HCP suspects that Caesarean section may camouflage a lack of good information and support before delivery as well as lack of access to pain control or doctors wanting to schedule births.
The highest rates of Caesareans in the world are found in Cyprus, Greece and Latin America (Brazil and Venezuela also close to or above 50 %).
Please note in the graph below that even though a Caesarean is costly, there is definitely no positive correlation between national wealth and high Caesarean rates; rather the reverse!
Source: WHO Health for All database, 2017-12-07 (poorly updated since 2016!).
Antibiotics consumption
There is shocking disagreement between different sources regarding antibiotics consumption.
EHCI 2016 therefore used the ECDC as data provider. The ECDC data does show the expected correlation with resistance data (indicator 3.6 above).
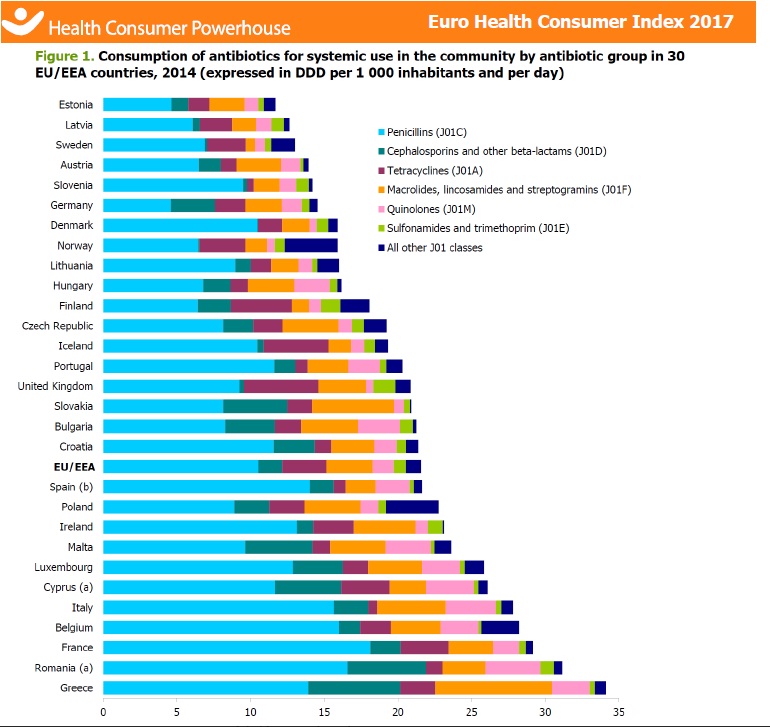
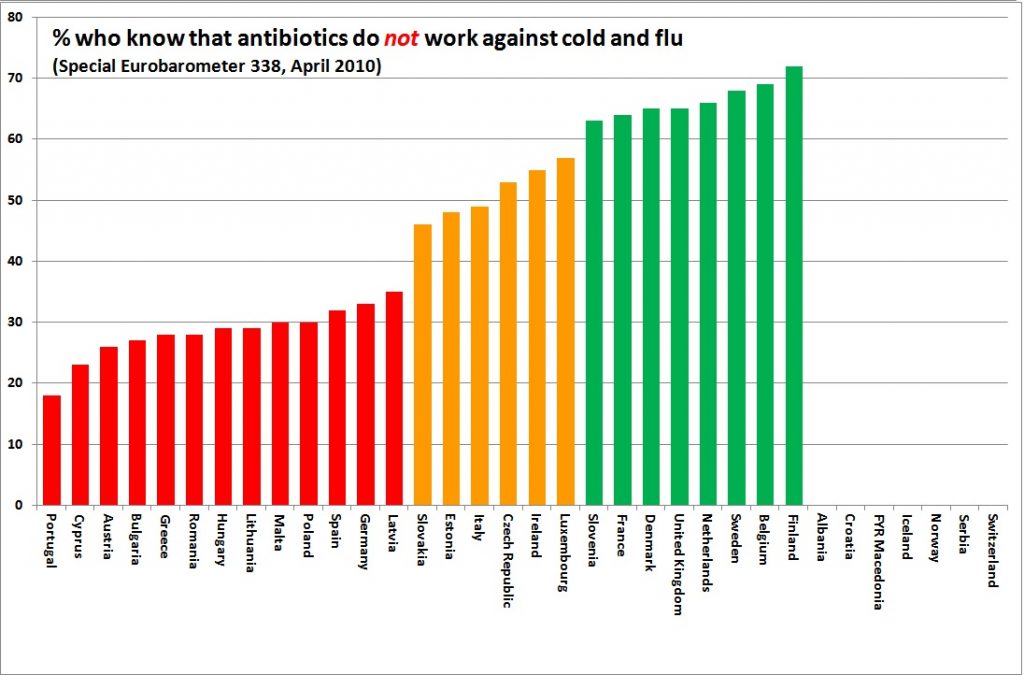
In 2012, the indicator used was “% of population who know antibiotics are not effective against cold and flu”. EHCI 2013 used actual per capita sales of antibiotics, with the assumption that a restrictive use is good from a resistivity point of view.
No sign of an EU healthcare role model – and maybe that is a good thing?
If the results of the Euro Health Consumer Index since more than ten years are studied, some conclusions could be drawn:
- European public healthcare keeps improving, counting treatment outcomes as well as the position of the patient/consumer.
- The correlation between money spent and healthcare performance is obvious for treatment results, but non-existent for Accessibility/Waiting Times.
- Major countries seem to benefit from purchaser-provider split systems (“Bismarck”). “Gosplan” single payer systems (“NHS”) seem manageable mainly in small countries, particularly if not fragmented by regionalisation.
- There are growing European mountains of healthcare data and statistics that are often used to successfully improve medical procedures. Little learning progress is made on health systems reform; doctors and some managers implement change, politicians and administrators more rarely do.
Once upon a time the HCP thought that the EU would play a role in advancing health systems performance to the benefit of Europeans. The cross-border care initiative could have become a powerful driver for care transparency and integration. But reality tells us that very little has happened.
The Euro Health Consumer Index points every year to a number of successful national initiatives; this year, to pick a few examples, how Slovakia radically has improved access to treatment, how tiny players such as Macedonia and Montenegro have used e-health to abolish patient waiting.
We wonder when Romania will climb up the index and score high up in the ranking. What is to be done? Who is willing to do it?
###
Thank you for your interest shown! If you find this useful, interesting or inspirational article, I invite you to leave your comment below or here.
For other articles and inspirational pills, check out our site or Facebook page.








Thanks for Sharing